Today we are launching Equivac® HeV, the world’s first commercially available Hendra vaccine for horses. This breakthrough is the culmination of a scientific journey that dates back to the emergence of Hendra virus in 1994.
Although the Hendra virus “disappeared” for some ten years (with only one case reported in 1999) after it was discovered in 1994, it has recently been identified every year in Queensland with serious consequences for the health of animals and people.
For my colleagues and I working at CSIRO’s Australian Animal Health Laboratory (AAHL), in Geelong, Victoria, and overseas, these outbreaks added urgency to our research on the Hendra virus.
The initial flurry of work following the emergence of the virus led to Australian mainland flying foxes being identified as the natural reservoir host of the virus.
Research waned somewhat towards the late 1990s, when a new virus – Nipah – emerged in Peninsular Malaysia. Nipah virus was linked to outbreaks of fever and encephalitis in people, and with respiratory disease in farmed pigs.
Nipah was rapidly identified as being a close relative of the Hendra virus, and there are distinct similarities between the two. They both have the ability to lead to fatal infections in several species of animal, as well as in people. And they infect animal and human cells in a similar way.
Following the terrorist attacks on September 11, 2001, the US Congress dramatically increased the level of funding for research into countermeasures – including vaccines and antiviral drugs - for perceived potential bioterror threats, such as Nipah virus.
In collaboration with researchers of the Uniformed Services University of the Health Sciences, Maryland, we generated, in vitro, one of the Hendra and Nipah virus proteins (sG) that’s essential for infection and showed that antibodies to this protein can block virus replication.
These observations – that the G protein provoked a strong immune response in naturally occurring Hendra and Nipah virus infections, and that development of antibodies to the G protein was associated with virus clearance in infected people and animals – suggested a vaccine based on the G protein antigen may be a feasible scientific goal.
The frequency of Hendra virus incidents after 2005, particularly the Redlands outbreak of 2008 and infections at Cawarral in 2009 in which two people died following contact with infected animals, brought the desirability of a vaccine for horses more urgently into the frame.
All human infections with Hendra virus have occurred following exposure to infected horses and direct contact with their bodily fluids. We believed vaccinating horses would provide an opportunity to break the chain of virus transmission from flying foxes to horses, and then to people.

Another benefit of a horse vaccine is that the horses themselves would be protected from a devastating infection that would otherwise most likely lead to their death.
As part of the ongoing research into countermeasures against biological threats, we’d developed the Hendra virus sG subunit vaccine with our US collaborators and tested it under laboratory conditions. The vaccine was formulated for use with an adjuvant (a substance that enhances the body’s immune response to an antigen) to enhance its efficacy.
Various forms of this preparation were evaluated in laboratory animals, where it was found to protect them from developing disease following exposure to Nipah and Hendra viruses and to prevent virus replication.
But a major hurdle to translation of this promising research into licensing for an equine vaccine was the lack of a commercial partner. This was a problem because the equine market is comparatively small, the infection problem largely confined to one state in Australia, and the public health impact of the disease is relatively insignificant compared to other illnesses.
Then, in 2010, a child received post-exposure treatment against Hendra virus infection after coming in close contact with an infected horse. This was closely followed by Queensland and Federal government funding to support the preliminary testing of the equine Hendra virus vaccine. This, in turn, acted as the catalyst for Pfizer Animal Health – our commercial partner - to join the research team.
The sG Hendra virus vaccine was soon formulated with a proprietary adjuvant suitable for use in horses. Early studies confirmed the development of immunity in vaccinated horses, prevention of disease following exposure to the virus, as well as the absence of viral shedding. This meant there was no risk of onward transmission to people or other susceptible animals.
In 2011, while this work was being undertaken, Australia witnessed an unprecedented spike in the number of Hendra virus cases in horses, in both Queensland and New South Wales. A total of 18 cases were identified. The first reported case of Hendra virus antibody detection in a dog outside of an experimental setting was also seen that year.
Intergovernmental Hendra Virus Taskforce was formed as a result, and additional funding was provided through the National Hendra Virus Research Program to ensure that the equine Hendra virus vaccine project was able to progress as rapidly as possible.
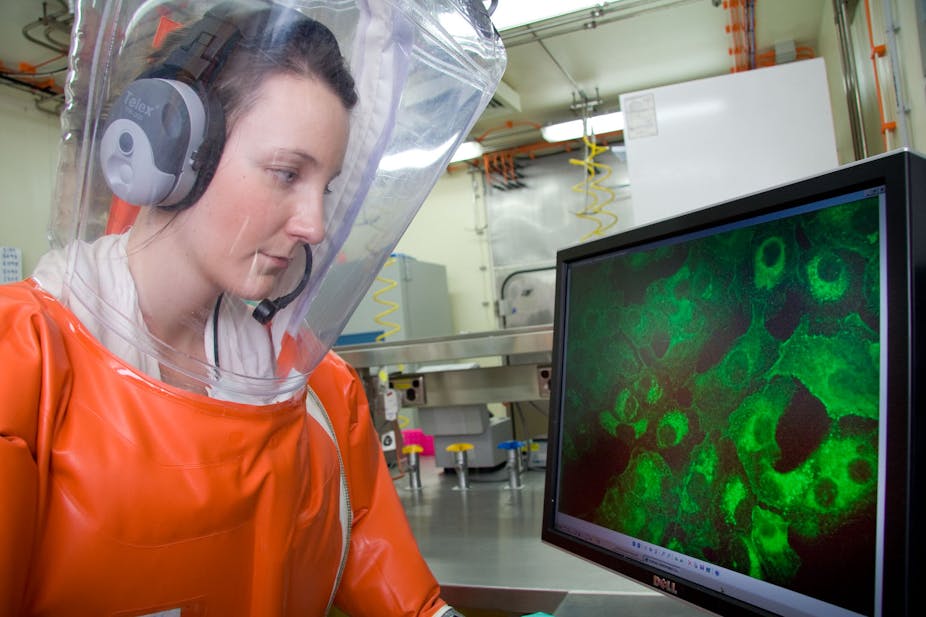
Optimising the vaccine presented additional regulatory challenges, as did undertaking efficacy studies in horses at the highest level of laboratory biocontainment. At times, progress seemed frustratingly slow. But in reality, the availability of a vaccine to protect horses from Hendra virus infection and, in turn, prevent the exposure of people to this disease, has been swift.
The Equivac® HeV vaccine is an important step towards breaking the transmission cycle of this disease, and reducing its impact on the horse-owning community. But it’s important to ensure that we continue to protect the health of our animals and people. And to do this, we need to maintain and continue undertaking research and adding to the tools in our armoury of weapons against the deadly Hendra virus.