Should you be denied life insurance or have to pay extra if you have a genetic risk for certain diseases? Should insurance companies even have access to your genetic data in the first place? This is known as “genetic discrimination”, a practice already banned in some countries, including Canada.
The Australian Treasury is currently working on a review of the relevant legislation, with insurance industry bodies arguing a total ban would raise life insurance bills.
But this legislation doesn’t just have implications for genetic discrimination. Genetic testing underpins vital branches of medical science. Our research shows the question of who can assess a person’s genomic data directly influences public trust in future genomic research in Australia.
What is genomic research?
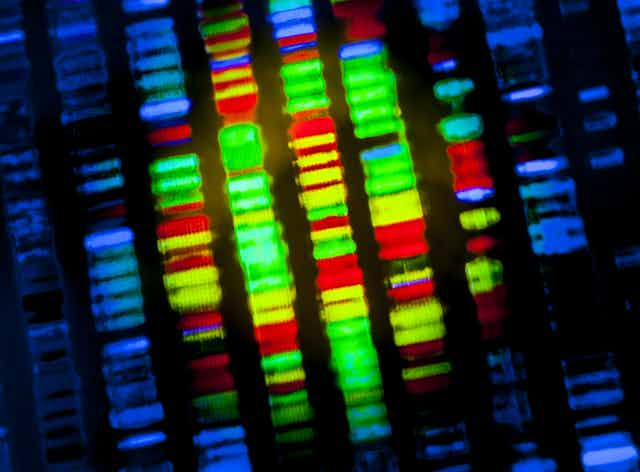
Human genomic research holds promise for the development of cures and treatments for cancers and heritable diseases. To achieve this, researchers rely on people willingly donating their genomic data. This is your DNA code derived from something like a blood sample. Genomic data is particularly useful when linked with lifestyle – diet, exercise, habits – and health records.
If researchers have access to this data from thousands of people, they can look for patterns to see if certain genes might be linked to certain illnesses or diseases. Treatments or cures can then be developed to target the gene or genes involved.
To assist with making genomic research viable and accessible for researchers, national-level biobanks exist, such as in the United Kingdom. These biobanks can store data from hundreds of thousands of people.
Australia does not yet have a national biobank, but some researchers in Australia do conduct studies that involve the collection of genomic data.
Can we trust biobanks?
Previous research has found people are generally supportive of genomic research and biobanks. They recognise the potential for new treatments or cures such research can bring.
However, trust in biobanks decreases substantially if there is any commercial involvement in biobank management or research. This poses a problem, as commercial involvement in biobanking is increasingly likely. Running these repositories, conducting research and bringing new treatments to market is expensive.
People who express such distrust often cite concerns that profit will be put ahead of the public good. One common issue is the perceived unfairness of “big pharma” hypothetically making large profits from freely donated genomic data.
Another primary concern, that is often a dealbreaker when it comes to hypothetically donating data, is that data will be sold to insurance companies who will then deny cover or increase premiums.
If people are unwilling to donate to biobanks due to the perceived risk of genetic discrimination from insurance companies, the scope of genomic research may suffer.
People are most trusting of biobanks if they are managed by universities and hospitals, who then also conduct the research. This is because these types of public institutions are not typically seen to be profit driven.

Would Australians trust a biobank?
Our research explored the required conditions for a trusted Australian national biobank. Specifically, we examined what Australians think about genomic research and sources of distrust. We also examined different legal safeguards that could be implemented to enhance trust and willingness to donate.
We started by surveying a statistically representative sample of 1,000 Australians. We found four groups Australians can be categorised into based on their attitudes towards genomic research:
- highly supportive and willing to donate to a national biobank (approximately 23% of the population if you extrapolate from our sample)
- supportive and open to donating but wary of commercial involvement (37%)
- supportive and open to donating but wary of commercial and governmental involvement (26%)
- completely unwilling to donate under any circumstances (14%)
In a follow-up study we interviewed 39 people from these groups. Across the four groups, including those who were willing to donate, there were clear concerns about genetic discrimination from insurers or employers. Concern about corporate profiteering was also widespread. However, respondents maintained a pragmatic view that pharmaceutical companies necessarily need to make some profit.
Based on the interviews, and a third experimental survey, it was clear a national biobank should be managed by a public institution. Additionally, we should have a data access committee comprising relevant experts.
This committee would assess applications from researchers attempting to access the data. For example, data access would be allowed only for researchers from established commercial or public organisations. Additionally, researchers would be compelled to only use data for ethical human health research and make no effort to identify donors.
Overall, Australians generally do support genomic research – they recognise its potential to give us much-needed new medical treatments and even cures.
But this support is undermined if people feel that genetic discrimination is a likely risk for themselves or their blood relatives.
Legislation that reduces this risk targets a main source of distrust that can make people unwilling to donate genomic data. A law preventing genetic discrimination could therefore indirectly benefit genomic research and support for a national biobank, should one exist in the future.
The author would like to acknowledge research collaborators Jarrod Walshe from Swinburne University of Technology, Dianne Nicol from the University of Tasmania and Mark Taylor from the University of Melbourne. The research project was based on a Medical Research Future Fund grant that was awarded to Professor Christine Critchley who sadly passed in 2020.