Scientific and medical articles, and websites by Crohn’s disease associations give similar definitions of the illness: “Crohn’s disease is a chronic, inflammatory disorder which may involve any part of the gastrointestinal tract from mouth to anus, however is mostly confined to the ileum and the colon.”
But what does this actually mean? And how does the disease affect its sufferer?
Crohn’s disease was first identified in 1623 by a German surgeon Dr. Wilhem Fabry, and later described (in 1932) by the American physician Burril B. Crohn. The cause of the disease is likely to be multifactorial – involving environmental, genetic and immunological factors – but it still remains unclear.
Some studies have recently shown that changes in gut bacteria may underlie the problem, predisposing certain people to the disease or initiating its symptoms.
Anatomy of the disease
Crohn’s disease is a form of inflammatory bowel disease (IBD). It causes the wall of the intestine to become inflamed, thick and swollen and may simultaneously or successively involve one or several gastrointestinal tract segments.
Usually, the disease involves the large bowel or colon (colitis), the part of the small bowel connected to the large bowel or ileum (ileitis), or both (ileo-colitis). Having “-itis” after an organ name means inflammation so colitis means inflammation of the colon. Involvement of the anus is common, affecting about a third of patients, but other parts of the digestive system, such as the oesophagus or the stomach are less often involved.
Patients often suffer unpredictable bouts of the disease, called flares, followed by periods of remission. But continuous chronic forms of the disease also exist. Crohn’s may stop progressing, particularly following effective treatment and the lesions it has caused in the gastrointestinal tract may be partially or completely repaired.
Clinical symptoms come and go unpredictably, and vary depending on the part of the digestive tract segment or segments involved (colon, ileum, anus, or whatever). Patients may experience cramping abdominal pain, diarrhoea (watery or bloody) and rectal bleeding.
Crohn’s can have other symptoms involving mainly the skin, peripheral joints (such as knees or elbows), the spine, the eyes or the bile ducts. Flares are usually accompanied with general symptoms, such as fatigue, loss of appetite, weight loss and fever, which are not specific to this disease.
Diagnosis and complications
Diagnosis at an early stage is rare – it’s often delayed because the general and non-specific symptoms often mislead clinicians. There’s no single and definitive test enabling a diagnosis of Crohn’s disease with complete certainty.
A diagnosis is made on the basis of detailed personal and family history, physical examination, laboratory blood tests (which may show inflammation in the blood), and examination of part of the bowel that can be performed either by endoscopic or radiological studies.
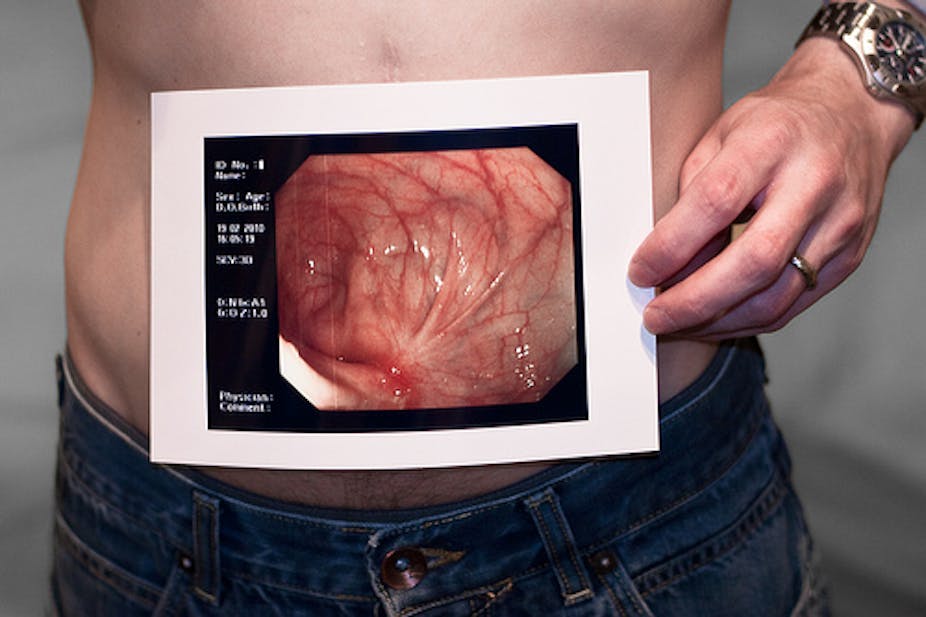
Endoscopy is direct inspection of the gastrointestinal tract with a flexible tube fitted with a camera that’s inserted through the anus or mouth. The procedure involves removing a small piece of tissue from the inflamed segment, which is usually performed to confirm diagnosis. Results from such tests will define whether a person is suffering from Crohn’s disease.
Although rarely fatal, complications related to Crohn’s disease may be serious. They include a narrowing of an intestinal segment (intestinal stenosis), which may lead to a block in the passage of intestinal contents (occlusion), perforation, abscesses, fistula (a tunnel connecting one loop of the bowel to another or to the bladder, or skin for instance), anal incontinence, venous thrombosis and cancer of the inflamed intestinal part.
The disease is associated with major morbidity, increased mortality, disability, economic loss, substantial psychological impairment and financial burdens. Not surprisingly, it has a significant effect on patients’ self-reported quality of life.
An autoimmune disease?
There’s some debate around whether Crohn’s disease is an autoimmune illness – where the body’s immune system attacks the body itself, destroying healthy tissue. Immune tolerance in the gastrointestinal tract is the result of a fine balance between immune cells that have the capacity to respond to gut flora (killing it and upsetting the balance) and regulatory immune cells making sure that this doesn’t happen.
But rather than being a true autoimmune illness with immune reaction against self tissue antigens, Crohn’s disease may reflect a breakdown in the normal immuno-suppression of gut immune cells, which then get out of control and react strongly to the gut flora. This, in turn, leads to a very severe inflammatory response with pathological consequences for the integrity of intestinal tissues.
Crohn’s disease equally affects both women and men, but it appears to be slightly more predominant in women in some studies. Prevalence also varies according to ethnic origins and countries. The highest incidence and prevalence have been reported in Northern Europe and North America.
Crohn’s disease starts mainly in adolescence and in young adults between 20 and 30 years of age, but may occur at any age. The largest risk factors are family history, followed by smoking. Smoking is not just an important lifestyle risk factor, but also a risk for aggravating the course of the disease.
Treatment options
Each clinical form of Crohn’s disease requires specific treatment strategies. Treatment is designed to prevent flares and reduce their severity and duration when they occur, helping maintain normal function, and preventing serious complications. And while there’s no specific medical or surgical cure, symptoms are treatable and can be controlled.
Short-term goals are to quickly control visceral involvement and weigh up the risks of immunosuppressive therapy. In the long term, the idea is to define the minimum effective treatment allowing remission and improving patients’ quality of life. Changes in lifestyle, such as stopping smoking, are an important aspect of controlling Crohn’s disease.
Drugs that suppress or modulate the immune system are usually prescribed as conventional therapy. Approaches involving artificial nutrition can be effective in certain cases. Surgery is performed when major complications arise such as perforation or stenosis, keeping in mind that surgery is decided as a last resort option due to the possibility of relapses.
In the absence of a cure, patients have to learn how to live with this condition. New treatments, such as biologics, have revolutionised the treatment of Crohn’s disease, leading to improvement of patients’ quality of life. Disease management is moving towards an increasingly more personalised approach as opposed to a one-size-fits-all broad immunosuppressive but toxic approach. And this is the good news.
See more Explainer articles on The Conversation.