Two views in today’s Medical Journal of Australia deal with attitudes to risk and economics, but with the added gravitas of a life-or-death outcome added to the consideration. The articles discuss the use of antibiotics in humans and animals, and whether the latter is having a negative impact on human health.
Antibiotics are one of the most important discoveries of the 20th century and have saved hundreds of millions of lives. Unlike money, which we seem to be able to print limitless amounts of currently, there are no new antibiotics coming down the pipeline.
The World Health Organization (WHO) has declared antimicrobial resistance, or “superbugs”, as one of the greatest threats to human health today. In the United States, United Kingdom and parts of Europe, there are mandatory requirements for hospitals to monitor and record hospital-acquired infections on a national database. Remarkably, there is no national database or antimicrobial resistance policy in Australia.
Researchers at the US Centres for Disease Control and Prevention estimated that in 2002, 1.7 million people in the US had hospital-acquired infections (where you go to hospital infection free, and pick up a superbug during your stay). Such infections add $4.5 billion to health-care expenses each year, and lead directly to 99,000 deaths.
In the MJA articles, Professor Peter Collignon, Director of the Infectious Disease Unit at Canberra Hospital and Stephen Page, a Veterinary Clinical Pharmacologist with Advanced Veterinary Therapeutics in Sydney, present their views on whether the use of antibiotics in farmed animals poses a risk to human health.
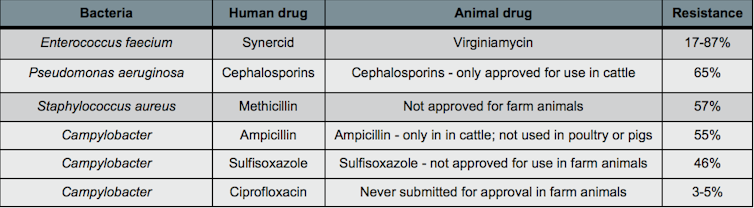
Collignon (the medic) and Page (the vet) disagree on a key point: whether the use of identical or near-identical antibiotics in our food chain is one of several contributing factors to the problem of antimicrobial resistance in humans.
Here it is important to separate the use of antibiotics for treating sick animals (veterinary use), and the daily application of antibiotics as “growth promoters”. Page argues that only 39 antibiotic agents are approved for use in farm animals in Australia, of which 6 are from classes with no human counterpart (this of course means that 33 are used in both humans and animal).
Australia imports approximately 700 tonnes of antibiotics annually; of this, 550 tonnes are used for either veterinary therapy (sick animals) or growth promotion (higher yields of growth of farmed animals). Of the 33 classes of antibiotics used in animal and humans, one third are classified as of high to medium importance in human therapy.
The Australian Joint Expert Technical Advisory Committee on Antibiotic Resistance (JETACAR), which was disbanded in 2002, found that antibiotic resistance could spread through consumption of animal products contaminated with a resistant bacterial strain, or via close contact with animals.
Significantly, for those antibiotics we’ve had the foresight to ban for animal use – as was the case with fluoroquinolones – there are very few superbugs resistant to that class of antibiotics in humans.
Collignon and Page both note that industry should be applauded for self-regulation here. The Australian Poultry Industry decided against using a third-generation antibiotic called cephalosporin in chickens, and the level of drug resistance in human infections is 3% in Australia, compared to more than 50% in countries using the drug.
Page adds that in Denmark, which has one of the most highly regulated policies for antibiotic use in the world, superbugs in animals are still a problem. Does this mean that such policies are ineffectual or that they decided to ban antibiotic use too late?
The Australian Department of Health and Ageing says “Australia’s food supply is one of the safest and cleanest in the world”. And we’re lucky to also enjoy access to a high standard of health care.
But while it is inhumane to withhold antibiotics for veterinary care of sick animals, we need to carefully rethink our attitude toward the risks of antibiotic use. With superbugs appearing more often in hospitals and causing more deaths, what risks are we prepared to take with human health by continuing to use antibiotics as growth promoters in animals?

